Pseudogynecomastia and Gynecomastia: What’s the main difference?
Psuedogynecomastia and gynecomastia are separated by only a few key differences among males. In both cases, there is excess fat or swollen tissue present in the chest region, leading to the appearance of breasts. Males of any age can develop either condition, but newborns, teens, and seniors are most susceptible.
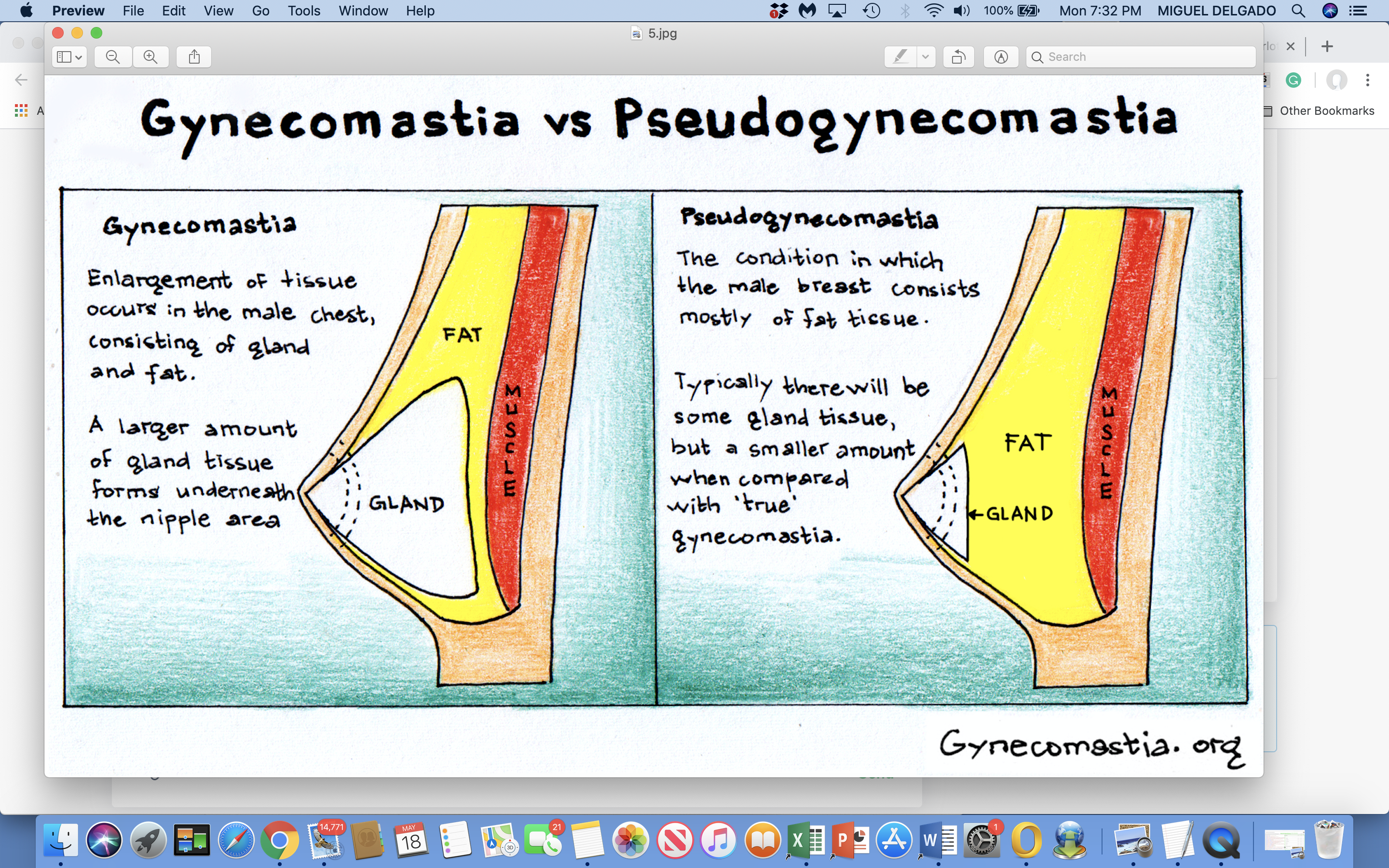
There is no difference in the appearance of breasts between patients with gynecomastia and those with pseudogynecomastia, but the type of tissue differentiates them. There is a number of potential causes of gynecomastia, which is characterized by excessive glandular and stromal tissue. In addition, pseudogynecomastia can be caused by excessive amounts of fat tissue.
There is no medical risk involved with either condition, however, many patients experience emotional distress due to gynecomastia or pseudogynecomastia, as well as issues with self-esteem and shame as a result of showing their bodies. In some cases, gynecomastia may indicate a more serious medical problem, so patients should also consult their general practitioner about possible causes. It is always best to check, even though this is a rare occurrence.
How to Understand Pseudogynecomastia
The condition of pseudogynecomastia is characterized by excess adipose (fat) tissue around, under, and behind the nips. In spite of the word “pseudo”, or something false or masked, “fake gynecomastia” is a very real disorder that can cause physical and psychological difficulties for some men. These physical and psychological issues are common to both pseudogynecomastia vs gynecomastia
Symptoms of Pseudogynecomastia
An appearance of bilateral enlarged breasts on the chest with excess fat.
The only thing that will feel firm is the excess fatty tissue below the chest.
The appearance of fat accumulation around the armpit region.
Pseudogynecomastia Causes
Obesity – Pseudogynecomastia is more straightforward, as it is a result of excess fat. Pseudogynecomastia occurs when a patient has excess chest fat deposition, and this shows up as enlarged breasts.
Treating Pseudogynecomastia
Weight loss is the first line of treatment for pseudogynecomastia. With the loss of body fat, your chest will also tend to become smaller. The majority of men lose weight and shape their chests through a combination of diet changes and increased exercise. Compression shirts are worn by some men to achieve the appearance of a leaner and flatter chest while they are losing weight. Even if a man reaches his goal weight, he may still experience pseudogynecomastia. Depending on the amount of residual fatty tissue and whether there is loose skin, the treatment may vary.
To treat pseudogynecomastia the fat deposits can be removed by liposuction alone or greatly improved by weight loss. In addition to liposuction of the residual fat, reducing (removing) a skin component may also be required to tighten the skin. Where the incision is placed will be determined by how much loose skin is present. Additionally, the areola is also reshaped to conform to the new chest contour. Many patients are concerned with the appearance and embarrassment of the areola (the darkly pigmented skin surrounding the nipple). The difference of treatment between pseudogynecomastia vs gynecomastia is liposuction.
How to Understand Gynecomastia
Pseudogynecomastia and gynecomastia differ primarily in the kind of excess breast tissue seen that causes them to appear enlarged and feminine. A male chest area with male breast enlargement will have excess glandular breast tissue (and possibly fat tissue as well). In comparison to fat tissue, the glandular tissue of the breast is firmer and more fibrous, and it does not respond to changes in diet or exercise. A hormonal imbalance is usually responsible for symptoms; however, certain medications (e.g., steroids) and illegal substances, such as marijuana, may also be responsible. These are the primary differences between pseudogynecomastia vs gynecomastia.
Symptoms of Gynecomastia
Gynecomastia symptoms include the following:
- Breast appearance with excess glandular tissue
- Nipples that are swollen or puffy
- Breast pain or tenderness in the areola
- There is a lump or disc of glandular tissue in the chest that is firm and hard to the touch
- A soft, fatty tissue may be present beneath the chest
- Sensitivity to touch or breast tenderness
Causes of gynecomastia
Hormones – Changes in hormone levels are frequently responsible for the development of gynecomastia. It can occur in a variety of ways. In newborn children with this condition, gynecomastia is caused by estrogen being passed onto the baby via the placenta. In general, hormone-induced gynecomastia in infants resolves over time. Puberty causes teenagers to undergo hormonal changes, and sometimes their testosterone levels drop so low that existing estrogen causes breast tissue to grow. Finally, older adult males are more likely to develop gynecomastia due to a decreased production of testosterone as a result of aging.
Medications – In certain cases, specific medications can contribute to the development of gynecomastia. Gynecomastia is more likely to occur in patients taking antidepressants, steroids, or medications for heart conditions, ulcers, or prostate issues. Antibiotics can also cause problems. In the event that medication contains estrogen or impacts estrogen levels, gynecomastia may result.
Alcohol and Liver Disease – Individuals who struggle with excessive alcohol consumption and suffer from cirrhosis are at higher risk of developing gynecomastia than their peers.
Thyroid issues: The thyroid gland, which is located in the throat, is a hormone-producing gland. Patients suffering from thyroid-related issues are occasionally affected by gynecomastia.
Narcotic Use: Narcotics, such as cannabis and heroin, are believed to be responsible for the development of gynecomastia.
Kidney failure – Gynecomastia can result from kidney failure although this is extremely rare. A physician should be consulted immediately if gynecomastia symptoms are present.
Testicular disease – Gynecomastia can occasionally indicate a serious testicular problem, including infection or cancer. Gynecomastia patients should seek medical attention if they experience various symptoms of testicular dysfunction.
Klinefelter syndrome – An extra X-chromosome is a characteristic of the Klinefelter syndrome. Gynecomastia can occur in patients with Klinefelter Syndrome.
For patients who are seeking treatment for their condition, it can be helpful to determine the source of their disease. There is a difference between gynecomastia and pseudogynecomastia in terms of causes.
Gynecomastia may have a number of causes, while pseudogynecomastia has only one.
Gynecomastia Treatment
The best treatment option for true gynecomastia is male breasts reduction surgery or gynecomastia surgery to remove the glandular tissue. In the course of the operation, the gynecomastia surgeon performs surgical excision techniques in order to remove the glandular tissue; your plastic surgeon may also use liposuction to eliminate fat tissue. You can remove excess skin and tighten the remaining skin if necessary to attain the desired chest contour.
The approach to treatment is typically performed by creating a small incision around the areola. Due to the small incision size and location, noticeable postoperative scarring is rarely a problem. The operative goal is to treat gynecomastia so the chest is contoured to a natural flat shape.
How to Know if You Have Gynecomastia or Pseudogynecomastia
Gynecomastia and pseudogynecomastia are both relatively easy to diagnose. Both of these conditions show up as excess tissue that appears breast-like on the chest. Gynecomastia and pseudogynecomastia are often recognized early on and cause men to harbor insecurity about their appearance.
Furthermore, these conditions are associated with other, less-recognized symptoms as well. In addition to the recognizable chest tissues, both gynecomastia and pseudogynecomastia have a number of symptoms that may confirm the diagnosis.
The pinch test is a common self-exam that you can perform to evaluate the tissue.